My Self-Recovery from Covid with Serious Heart Risk
This is a story of how I recovered from Covid while previously having a major heart reaction to my second Moderna vaccine. I am not a doctor, and this should not be taken as advice, but rather my personal story of how I beat Covid with a serious heart issue without ending up in the ER (again).
Backstory – My Heart Attack after Moderna Vaccine
In 2021, I took my second Moderna vaccine. Four days later I had intense chest pains. Not knowing what it was, I took ibuprofen to sleep and decided if it was still painful in the morning I would drive myself to the hospital. It was, and I went in the next day. After a 30 minute wait in an empty lobby they did an EKG and diagnosed a heart attack. At that point things happened quickly. I was taken by ambulance to a bigger hospital (Lee Healthpark, Ft. Myers), where the doctor wanted to perform a cardio angiography right away. This is the gold standard for detecting obstructions in arteries and veins around the heart and involves a wire physically inserted into an artery that is pushed into the heart where die is injected. The die is imaged by continuous xray. The entry point was my wrist.

Figure 1. Wrist entry point for an expensive cardioangiography. A wire was inserted from this point through the artery into my heart for direct visualization of obstructions. As a healthy, 46 year old, non-smoker, I had no obstructions.
I am convinced that medical practice in the US has become administratively overburdened, yet medically inflexible and dangerous. It’s focus is on risk management for hospitals over patient care. If there is a conflict between these the hospital wins. Doctors must follow a script provided by insurance companies for exact steps on the order of procedures. This makes obsolete any discussions with the patient about history or sensation. I told the doctors that I was physically fit, age 46, never smoker, exercise regularly, and the chance of an obstruction was extremely low. The cardio doctor suggested the $25,000 cardioangiograhy as my only option. I don’t believe he was seeking to understand the whole problem, just this narrow aspect of possible obstruction related to his area of expertise despite how unlikely. I think he enjoyed preforming the procedure, referring to his cardo ER as a “racing pit”, and his team as a “pit crew”, which has the effect of objectify the patient as.. a car (rather than a person). The cardioangiography showed no obstructions.

Figure 2. Echocardiogram performed the following day. This procedure could have been done first, and might have revealed something if observed before nitro medication.
An echocardiogram could have been performed first but wasn’t. This was done the following day. At the time I was diagnosed with Takotsubo cardiomyopathy, and this non-invasive test may have been able to identify the Takotsubo cardiomyopathy early. Interestingly the classical heart shape for Takotsubo was not observed in the echo on the next day. I am convinced that doctors really do not understand the heart effect of Covid or Covid vaccines. I had no better understanding of what happened.. and was sent home with Tylenol.
I believe Covid upsets the medical protocols of insurance companies and hospitals. It is not well understood, while defying the modernized flow-chart approach to medicine.
That’s how this all started. A non-obstructive heart attack, despite not seeing the classical octopus shaped heart muscles in an echocardiogram done the following day, although the heart attack may have passed by this time. I was considered high risk for complications and told the benefits of further boosters we too risky for me.
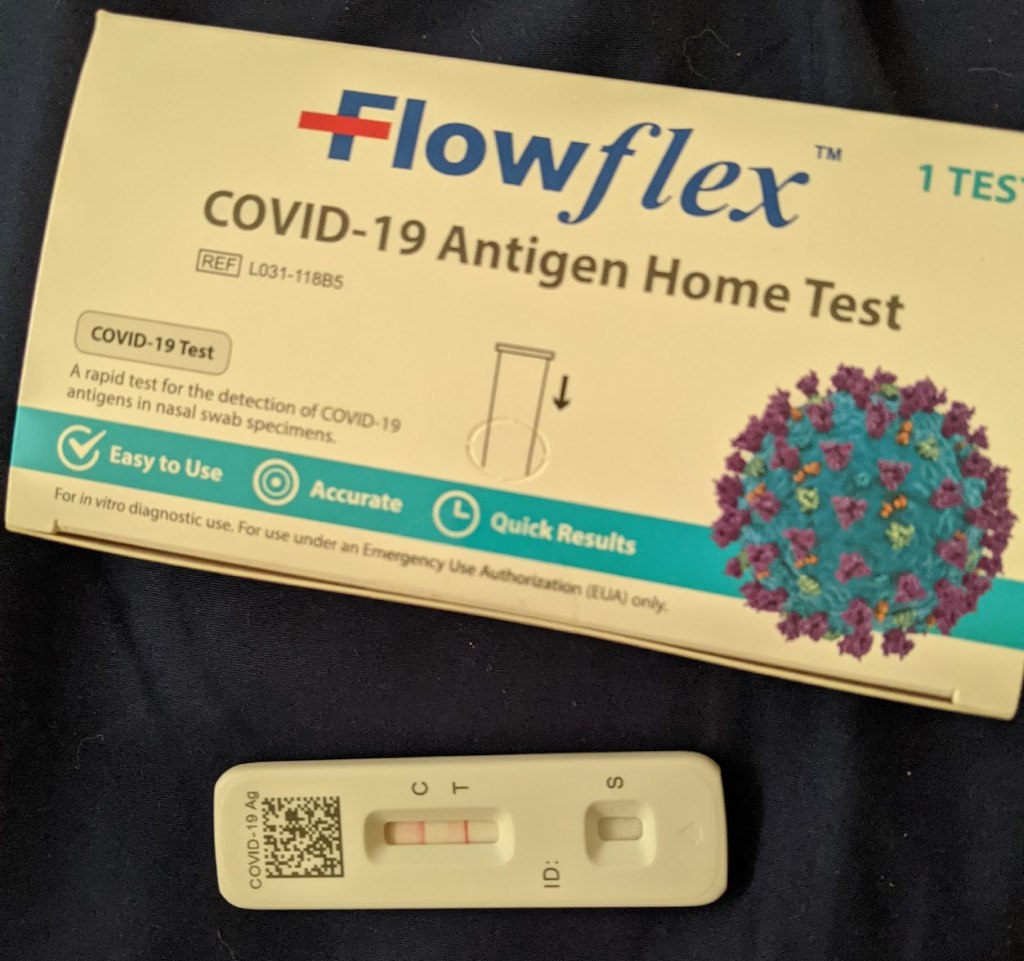
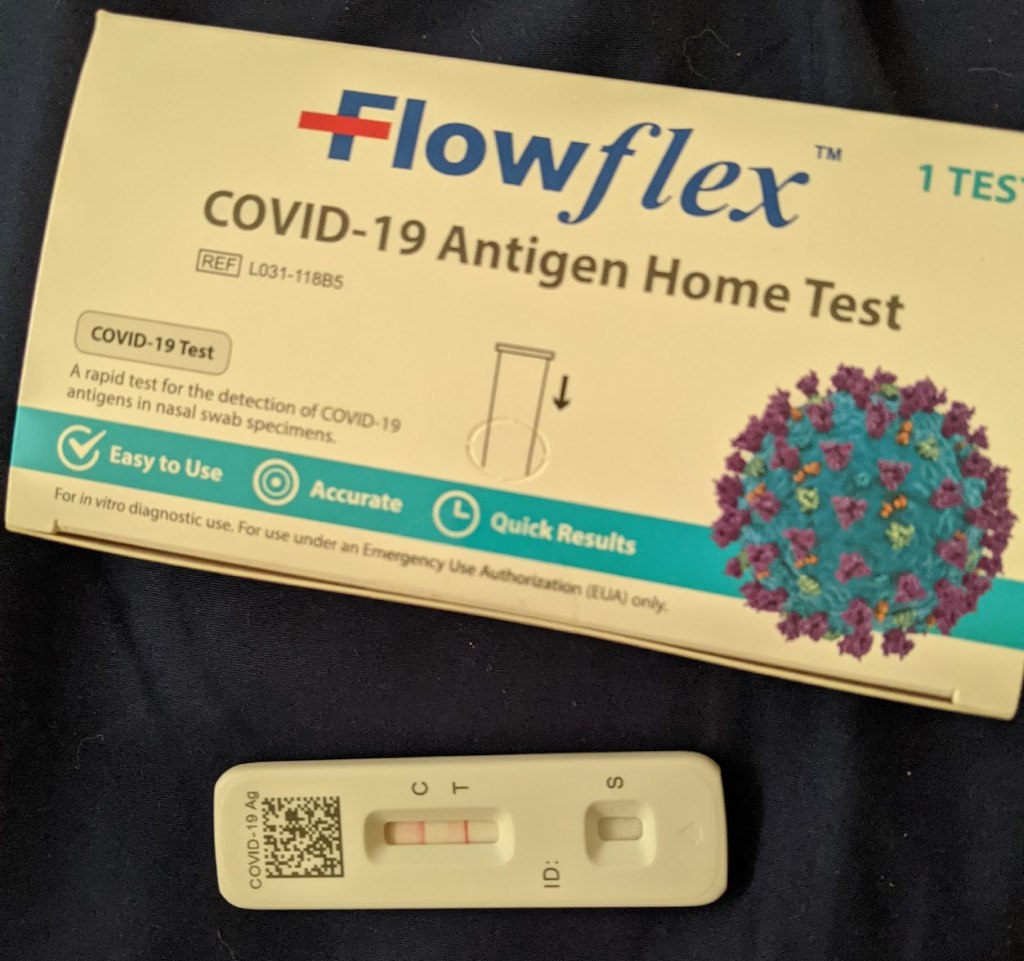
Figure 3. Positive Covid-19 FlowFlex test on January 8th, 2023.
My Self-Recovery from Covid with a Serious Heart Risk
But this story is not about my heart condition, its about how I recovered from Covid without ending up in the ER again. Using actual knowledge and what I believe doctors should do.
I was able to avoid Covid for two years. Then on Jan 8th, 2023 after feeling extremely sick, I tested positive for Covid-19 (FlowFlex rapid test). I knew it was real because my heart rate jumped to 135 bpm and didn’t come down for the entire day. I felt extremely cold, chills, had a fever, and felt worse than any sickness I had experienced before.
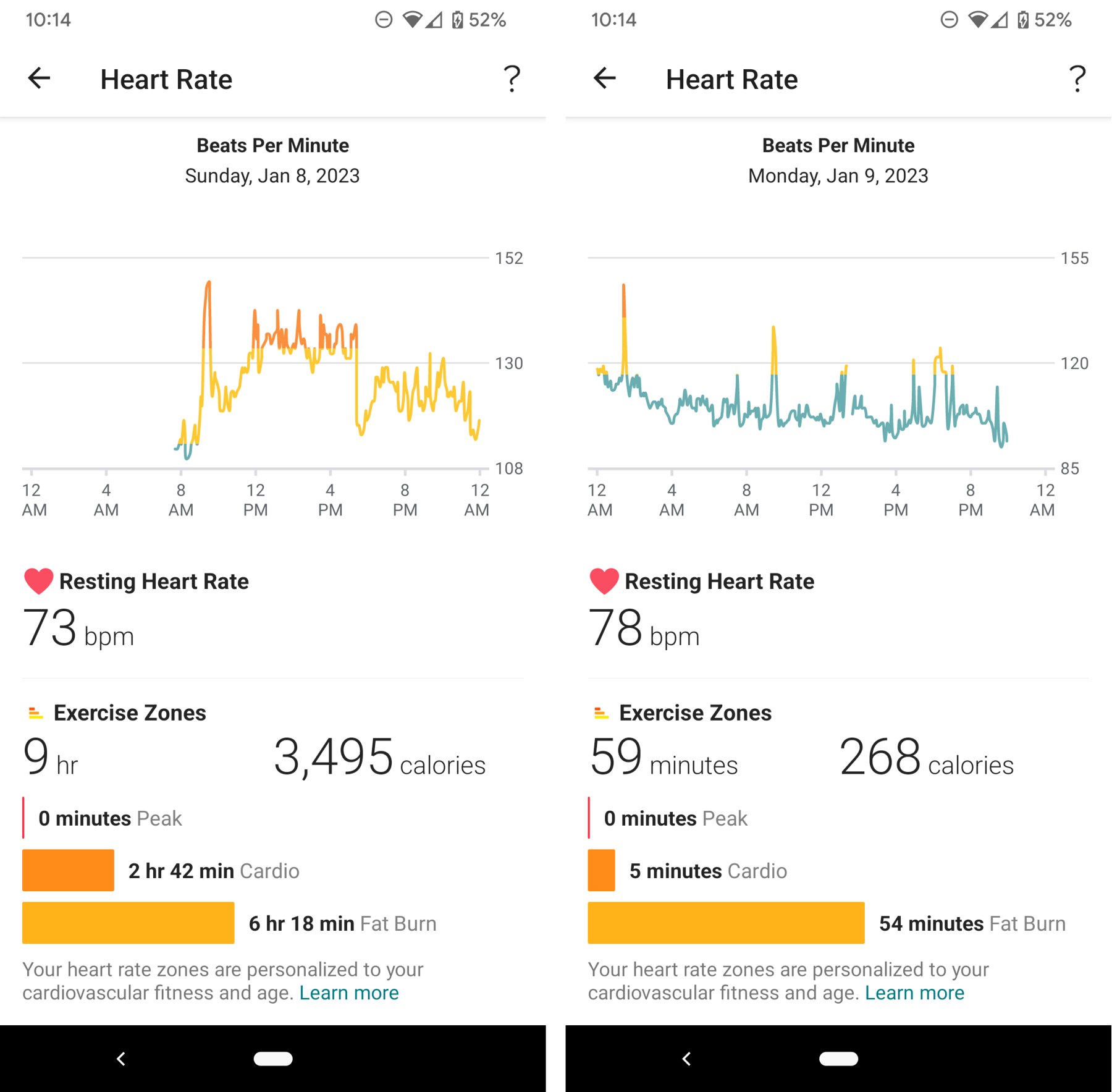
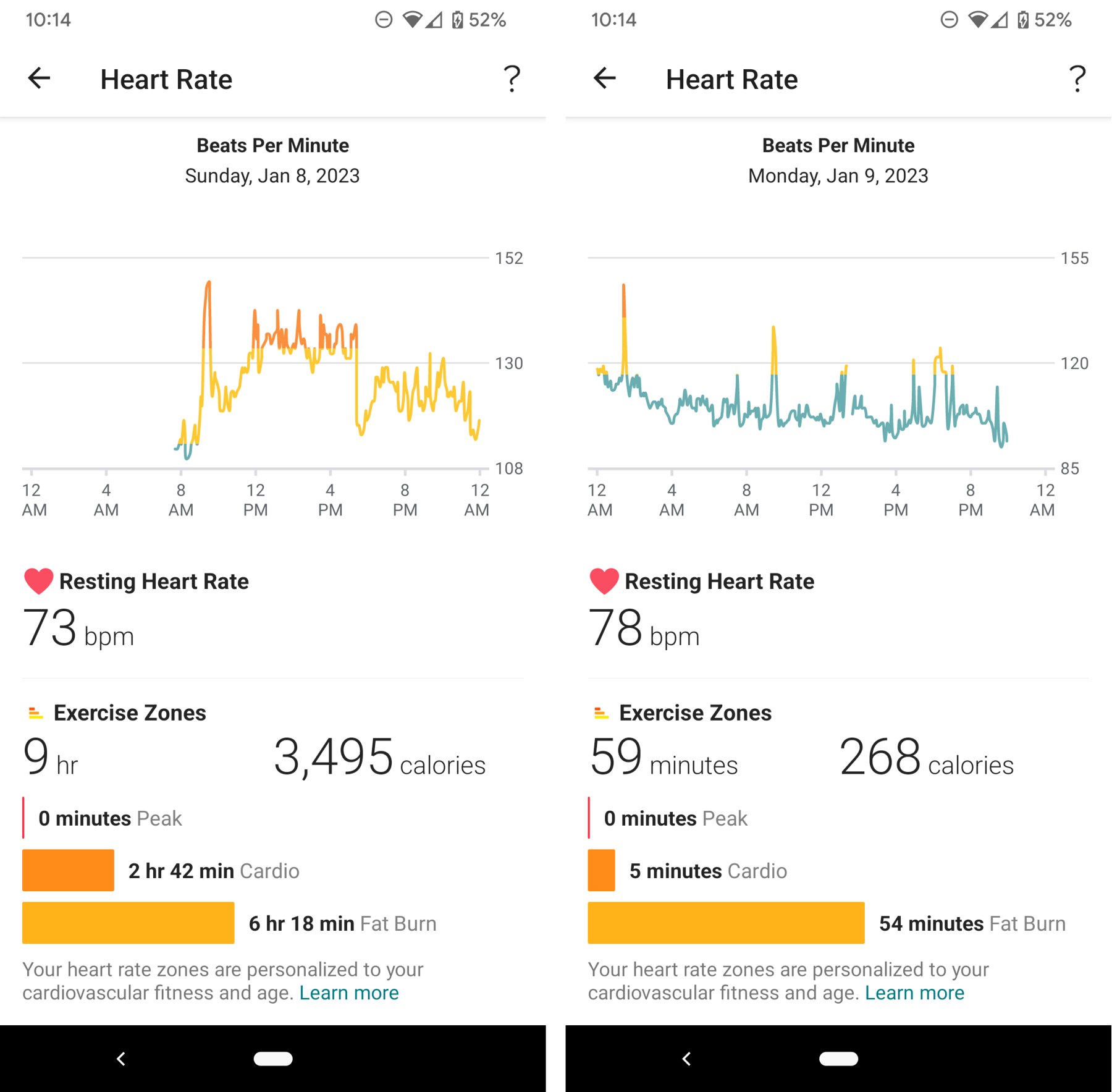
Figure 4. A FitBit tracker shows my heart rate on my first day of Covid-19 (left), and the gradually decline in peak heart rate the following day (right). In the left figure you can see that my heart rate peaked at over 145 bpm and remained above 130 bpm throughout the day despite the fact that I was doing nothing more than sleeping or laying in bed.
I knew that I had to rest my heart immediately, and with two blanket layers, went to sleep for 14+ hours.
Why not the ER now? I was at high risk. Yet, I did not have chest pains (like before) and I knew if I could calm my heart that would be heading in the right direction. I didn’t yet feel an emergency was happening. Despite feeling crappy, having no appetite, unable to do anything standing for even 10 mins, I knew that everything must focus on relaxing and maintaining my heart. It must rest and recover.
Here’s what I learned for myself..
Fresh air is absolutely essential. The purpose of the heart is to move oxygen, from the lungs to the rest of the body. Covid is making that harder. Pulmonary cough even more so. More oxygen allows the heart to work less hard. I fully opened the window in my room, both day and night. I kept this as a hard rule. Oxygen!
Understanding oxygen in air: https://www.ictinternational.com/casestudies/understanding-oxygen-in-air/
Globally the air holds 21% oxygen on average. Humid air, such as in Florida, holds less oxygen. The percentage reduces to 18% oxygen in air when the relative humidity is over 80%. The oxygen percent drops another 2% if the temperature goes over 100 degrees. So on a hot, humid day, the oxygen in air is doubly reduced.
Did you know that your own exhaled CO2 builds to impairment levels when sleeping in a fully closed, non-ventilated room?
Sleeping closed room indoor CO2 analyzed: http://vair-monitor.com/2016/09/29/sleeping-closed-room-indoor-co2-analyze/
Indoor carbon dioxide levels could be a health hazard: https://www.theguardian.com/environment/2019/jul/08/indoor-carbon-dioxide-levels-could-be-a-health-hazard-scientists-warn
CO2 is measured in parts-per-million (ppm) and just 1000 ppm can cause impaired thinking, while 5000 ppm is considered dangerous. CO2 can easily rise above 1000 ppm at night in an unventilated room. A ceiling fan does not help because it just circulates the air rather than bringing in fresh air. I needed as much oxygen as I could get! The windows stay fully open.
Proper tools. I knew this would not be a typical Covid recovery. The heart is a subtle thing that we aren’t usually aware of – hence the study of medicine. I knew that I could not rely on my “feeling” or sensation alone for something so critical as my heart. Here is what I had or acquired:
Fitbit watch ($100) – Continuous monitoring of heart rate during day and night, extremely valuable.
Wrist BP monitor ($40) – Check BP as needed
Finger Pulse Oximeter ($22) – Measure oxygen efficiency in the blood.
These aren’t proper tools by medical standards but they are for my use. That is considering both the quality and cost. A Fitbit watch and wrist BP used correctly perform the main tasks I needed them to – measuring how hard my heart is having to work.
I consider these essential tools for monitoring the heart. One could have a heart rate of 80 bpm yet a blood pressure of 150/100 or 100/60 would be dangerous. Together heart rate and BP tell me how hard my heart it working. To make the heart work less, it’s all about the oxygen, so the PulseOx measures that conversion efficiency of the lung as a percentage of oxygen bound to the blood. I could determine what to do based on these measurements rather than a guess or feeling.
Don’t exercise. There is a school of thought that says you should do light exercise during Covid recovery. With a heart condition the conclusion I came to is don’t!. Just a few minutes walking pushed my heart rate to 120-130 and made me feel faint. Give it time, let my heart heal, let it recover and let my body learn how to deal with Covid. Rest first above all else.
Temperature regulation. With the window fully open for oxygen, I needed to control my temperature. In January in Florida it was cold at night but hot during the day. Two heavy blankets worked well, that I could layer or unlayer as needed. This helped drop my fever.
Cough control. Coughing is a difficult issue because it may be a lack of oxygen causing the cough (dry cough). Combine that with a pulmonary infection and it could make it very difficult to breath and sleep (mucus producing cough). I found the most important thing is don’t bury my head in the heavy blankets. While comforting, there’s no oxygen under a blanket. When I sleep on my side, I feel my lungs are compressed, and the cough is worse because airways are blocked. So I learned to sleep on my back, lungs flat, even if I do turned my head to the side. Pushing the blanket close to the side of my head, but not obstructing my face, helps me to feel I am sleeping sideways even though my back and lungs are laying completely flat. If I need even more air, I stretch my head up, making a straighter airway to my lungs.
Lots of water. With heavy blankets, I was sweating profusely. The FDA recommends that men drink a full 3.7 litres (1 gallon) of water per day when we are healthy!. Despite how abhorrent anything tastes, even water, I knew that I needed to drink at least a full gallon every day. One day I missed a water session before afternoon nap and and woke up incredibly dizzy, that was the closest I came to thinking a heart attack was imminent (but still no chest pains). But I drank water and laid down immediately. If I felt incredibly terrible at any time, it was most likely water, and drinking two glasses usually resolved it.
Food. This is tricky because I had no appetite and knew that some foods would just make me sick. I found that the best were fresh fruits (containing more water) and some soups. Others have suggested gatoraid and green tea. Gradually I found I could add more foods to build strength, and this made sense as I recovered.
Tylenol (acetaminophen). I now accept no other pain meds due to my heart condition. Ibuprofen, Tramadol, etc. all have possible heart interactions that can raise or lower blood pressure. Not taking any chances. Tylenoln is know to reduce pain while also stabilizing heart rate and pressure. If I have trouble sleeping due to a cough, I take Tylenol.
Careful self-monitoring. During this entire time I was monitoring my heart closely. What was my heart rate?, my blood pressure?, my PulseOx? Were they in reasonable ranges or at least getting better? Did I feel any acute chest pain that might suggest a heart attack? Everything was focused on easing the stress on my heart, first with fresh air/oxygen, then with limited activity and plenty of sleep. Everything else was secondary despite how uncomfortable it was.
Fortunately this careful approach worked for me. On day 1 of my Covid recovery my heart rate stayed at 135 bpm the entire day and even while sleeping, yet with normal BP. My Fitbit recorded a 17 hour sleep, that must be some kind of record. On day 2 my heart rate averaged 100 bpm including during sleep, where my typical nightime heart rate is 65-70. So I knew that my heart was still working too hard. However, it was still dropping, by day 3 my heart rate dropped to high 90s.
I felt a bit better at this point, but if I tried to get up a do something even for 10 mins my heart rate would jump to 140 bpm. I wasn’t in the clear yet. I knew that I just need more rest and sleep until my body could figure out how to fight Covid and my heart could get back to normal. It’s all about oxygen, rest, and water. I had two rounds of Moderna vaccine so my outcome should be better than being unvaccinated.
Reflections on our Medical System
I truly shudder to think what would have happened if I went into an ER.
Do I think any of the above things would have happened in a calm, considerate way, focused on these basics and easing patient stress toward healing?
Not a freaking chance! My own past experience has shown, repeatedly, that hospitals are about efficiency and risk mitigation and I don’t see any efforts in the medical community to address these fundamental failures. I believe the most important factors in my recover were oxygen and decent rest. In an ER oxygen would be administered directly but good rest depends on comfort, lack of interruption and calm – things that ECU (Emergency Care Units) at hospitals often forgo due to risk management practices – hourly blood draws, cold rooms, excess lighting, monitor noises. Science-based methods, flow chart medicine, nurse shortages, and rising patient numbers have nearly eliminated the concepts of patient dialog and comfort as factors in care and recovery (unless you have money). Understaffing makes these challenges more difficult.
Back in 2021, the doctor who did the original wrist-entry cardioangiograhy, asked me to stay overnight in the hospital to monitor me. My heart attack symptoms and chest pains were reduced earlier that day due to use of nitrous meds. However, after the tests he “forgot” to prescribe any pain meds that evening, and I woke up in the hospital at 2am with the same chest pains that I went in with during the heart attack. It took 2 hours to find, and get approval (?), from another doctor to get new chest pain meds – I was probably having another heart attack. Meanwhile I was in a cold room, with thin blankets, while nurses woke me every 2 hrs attempting to draw blood from shivering vein-constricted fingertips, because I was told that two easily accessible IVs put in earlier could only be used by the doctors. Can we not invent a machine that pulls a small amount of blood through an IV while you sleep and tests it discretely? Why draw blood so frequently? Risk management. I believe overnight stays in the ECU are only there to prevent a major emergency, but may in fact make the situation worse since that don’t focus on symptoms and recovery. In my experience it wasn’t for care; I didn’t sleep at all due to the cold and failed blood draws.
I was only able to talk to the cardio doctor a total of 15 mins, 5 mins when he first insisted on the cardioangiography and 10 mins when they sent me home with Tylenol. My impression is that he didn’t really listen to a single thing I said.
Doctors wonder why patients take to self-learning and online knowledge. The reason should be very clear, our medical system is failing the patient in favor of the hospital, the insurance company, and the system. Patients in the US deserve a better system. Listening, patient care, comfort, history and communication should happen with science and risk management, not exclusive to these.
This recent story began when I went on a two week trip over the 2022-2023 new year, for me, a long time to be away from my 15-month old daughter Camellia. Covid was diagnosed by rapid test toward the end of my trip. When I came back I went directly into home quarantine for Covid. She wasn’t even aware I was back, since my room door was closed, and I kept quiet not wanting her to be exposed to me. She doesn’t know I am here, but I know she is there. I can hear her playing.
Update:
On April 21st, 2023 I experienced a very serious episode of food poisoning. I had vomited six times, and woke up at 2am with a heart rate of 170 bpm, and extreme sweating. Whereas my actual Covid-19 positive sickness from January 2023 had resulted in a serious cough and high heart rate, I did not experience chest pains at that time. However, during this food poisoning in April 2023 the chest pains were extreme. I am familiar with digestive-related chest pains, which feel like a pressing, bubbly pain from the stomach upward. This chest pain occured a few days after the primary sickness. The chest location was much higher, in line with the clavicles, and spreading across the chest from the center. The chest pain was intense enough to cause dizziness and blurred vision. Yet my heart rate and blood pressure had dropped to normal by this time. I am suspicious that these chest pains may be a form of long term Covid, where any type of sickness will induce a heart-attack like chest pain.
The question for cardiologists is this: What could cause an upper chest pain and dizziness yet not be a heart attack? Is there the possibility that long-term Covid-19 symptoms could cause this, and if so what are the mechanism and proper treatment?
PS. I am not against medical science per se, and especially the modern benefits of technology and medicine. This article calls out specific systematic practices by insurance companies, hospitals and by doctors that have, in an extreme sense, shifted away from actual patient care and recovery.